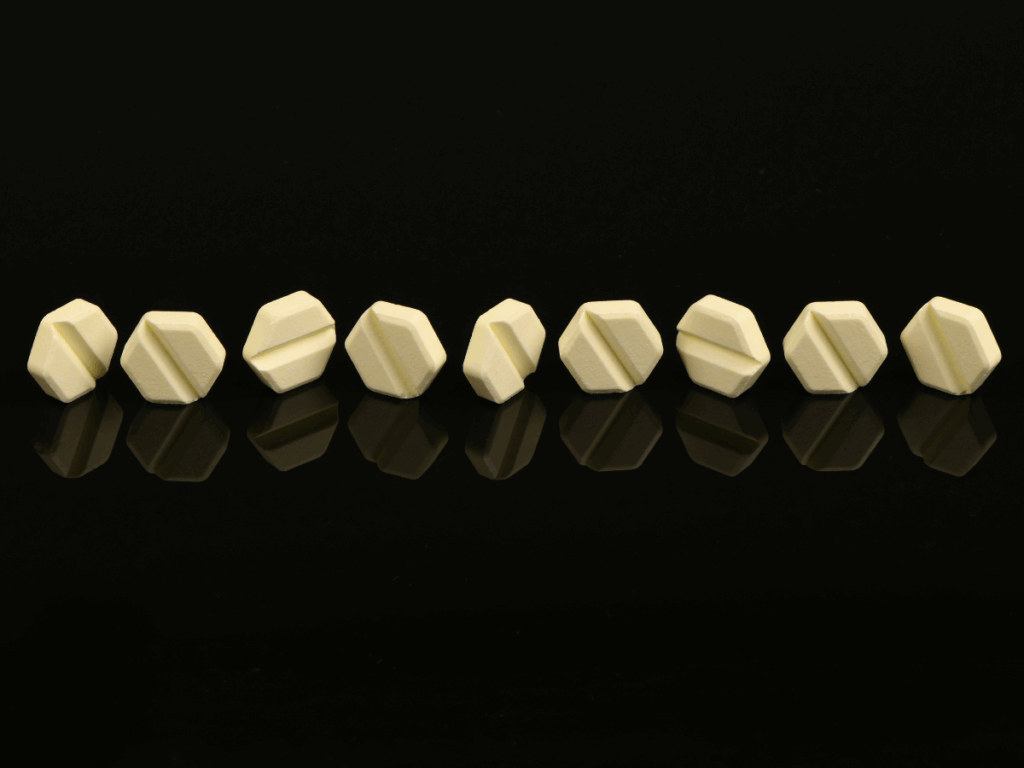
What Are Benzodiazepines?
Benzodiazepines (often shortened to “benzos”) are prescription central‑nervous‑system depressants used to treat anxiety disorders, insomnia, muscle spasms, and seizure conditions. Popular brands such as Xanax (alprazolam), Valium (diazepam), and Ativan(lorazepam) work by amplifying the calming effects of the neurotransmitter GABA, producing rapid relief from tension, racing thoughts, and sleeplessness. Because their benefits appear quickly, most prescriptions are intended for short‑term or intermittent use. When benzos are taken in higher doses, for longer periods, or in combination with alcohol or opioids, the same properties that make them therapeutic can trigger tolerance, dependence, and, ultimately, addiction.
Recognizing Benzodiazepine Misuse and Dependence
Benzodiazepine misuse is clinically recognized within the DSM-5 under the broader category of Sedative, Hypnotic, or Anxiolytic Use Disorder. This condition is characterized by a persistent pattern of use despite the occurrence of harmful consequences, including emotional, cognitive, or behavioral effects. Red flags may include escalating prescriptions, daytime drowsiness, memory lapses, neglected responsibilities, and social withdrawal. With nearly 10,000 overdose deaths annually involving benzodiazepines, often alongside opioids, early recognition and compassionate, medically informed intervention are essential to preventing further harm.
What Makes Benzodiazepines Addictive?
Benzos bind to special sites on the GABA‑A receptor, “super‑charging” GABA’s inhibitory signal and flooding the brain with a sense of tranquility or even mild euphoria. Repeated exposure forces the nervous system to compensate; neurons fire more vigorously when the drug is absent, driving both tolerance and distressing rebound symptoms. The fear of that rebound—rather than the pursuit of pleasure—often locks people into continued use.
Biological Factors
- Tolerance & Neuroadaptation: Continuous dosing reduces natural GABA activity, so ever‑larger amounts of the medication are needed for the same effect.
- Genetic & Medical Vulnerabilities: A personal or family history of substance use, chronic anxiety, or sleep disorders can accelerate progression to dependence.
Psychological Factors
- Emotional Coping: Many patients begin relying on benzos to blunt stress, trauma, or grief, reinforcing use whenever discomfort arises.
- Environmental Cues & Co‑Use: High‑pressure lifestyles, social circles that normalize pills, or combining benzos with alcohol intensify psychological attachment and complicate quitting.
How Does Benzodiazepine Affect the Brain?
By amplifying GABA, benzos swiftly dampen activity in the amygdala (fear center), hippocampus (memory), and brainstem (vital functions), slowing thought processes and body rhythms. While helpful short‑term, chronic exposure erodes the brain’s own ability to regulate mood and alertness, and can trigger paradoxical anxiety, irritability, or aggression when the drug wears off. Over time, the nervous system becomes hypersensitive to stimulation, making abrupt discontinuation hazardous.
Short / Long‑Term Effects on Brain
- Short‑Term: Reduced anxiety, sedation, slower reaction time, impaired short‑term memory, and decreased coordination.
- Long‑Term: Persistent cognitive clouding, difficulty learning or concentrating, emotional blunting, increased depression, and—in rare cases—benzodiazepine‑induced psychosis.
How Does Benzodiazepine Affect the Body?
Systemically, benzos relax skeletal muscles, slow gastrointestinal motility, and depress respiratory drive. Their sedative properties magnify the effects of other depressants, which is why poly‑drug misuse is particularly dangerous. Even therapeutic doses can cause next‑day drowsiness, increasing the likelihood of accidents at work or on the road.
Short / Long‑Term Effects on Body
- Short‑Term: Drowsiness, slurred speech, dizziness, blurred vision, decreased blood pressure, and impaired motor control.
- Long‑Term: Physical dependence, rebound insomnia, suppressed breathing during sleep, weight fluctuations, increased risk of falls, and potential fetal harm if used during pregnancy.
Overdose Risk
Acute benzodiazepine overdose may produce profound sedation, hypotension, respiratory depression, or coma. The danger multiplies when benzos are combined with opioids or alcohol—most fatal overdoses involve at least one additional depressant. Emergency care and, when appropriate, administration of flumazenil (a benzodiazepine antagonist) can reverse effects, but careful monitoring is essential to prevent recurrent sedation or seizures.
Benzo Withdrawal Symptoms
Because benzos alter neural excitability, sudden cessation unleashes a surge of over‑stimulation. Early symptoms include anxiety, tremors, sweating, insomnia, and nausea; severe cases can escalate to hallucinations, delirium, or life‑threatening seizures. Withdrawal typically peaks within the first week, but lingering sensitivity—called protracted withdrawal—may persist for months. A medically supervised, gradual taper is the gold standard for reducing risks and discomfort.
Treatment Programs for Benzodiazepine Addiction
- Medically Supervised Detox: Recovery begins with a comprehensive assessment and a customized tapering schedule—often substituting a long‑acting benzo like clonazepam or diazepam and reducing the dose slowly. Inpatient settings provide 24/7 monitoring for people with high‑dose use, co‑occurring disorders, or prior withdrawal seizures.
- Inpatient & Residential Care: These programs remove external triggers, deliver constant medical oversight, and integrate individual therapy, group counseling, and holistic activities (yoga, art, mindfulness) to rebuild healthy routines.
- Intensive Outpatient Programs (IOP): For milder dependence or step‑down care, IOP offers multiple therapy sessions per week while clients live at home, balancing flexibility with structured support.
- Evidence‑Based Psychotherapies: Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Motivational Interviewing (MI) help patients confront underlying anxiety, challenge catastrophic thinking, and learn non‑pharmacological coping skills. Contingency management reinforces abstinence with tangible rewards.
- Medication‑Assisted Support: Although no drug is FDA‑approved specifically for benzo addiction, non‑addictive medications like SSRIs, SNRIs, buspirone, gabapentin, or pregabalin can ease persistent anxiety and improve sleep during and after tapering.
- Peer & Family Support: Groups such as Narcotics Anonymous (NA) or SMART Recovery provide community and accountability; family therapy repairs relationships strained by addiction and educates loved ones about healthy boundaries.
- Relapse‑Prevention Planning: Every discharge plan should map out triggers, coping strategies, emergency contacts, and regular follow‑ups. Celebrating milestones, pursuing purposeful goals, and staying engaged in therapy or support groups dramatically improve long‑term outcomes.
With compassionate, multifaceted care, individuals can break free from benzodiazepine dependence and reclaim a balanced, fulfilling life.
Begin the Journey Back to Calm
If you or someone close to you is navigating benzodiazepine dependence or facing the challenges of withdrawal, you don’t have to do it alone. Compassionate, expert care is always within reach. Our team is available 24/7 at (888) 534-2295 to help you access safe, medically supervised detox and personalized treatment options designed around your needs.
Not sure where to start? You can verify your insurance online or speak directly with one of our specialists in confidence. We’re here to guide you through every step, offering trusted tools and clinical insight so you can move forward with clarity, confidence, and peace of mind.
Reaching out may feel daunting, but it’s also an extraordinary act of courage. It marks the beginning of a healthier, more centered life—one built on healing, trust, and sustainable recovery.
Immediate Help and Support
Whether you’re ready for treatment or simply gathering information, these resources are available to support you:
- Legacy Healing Center: Call (888) 534-2295 to speak confidentially with a specialist in benzodiazepine detox and recovery.
- SAMHSA National Helpline: Dial 1-800-662-HELP (4357) for free, 24/7 support and treatment referrals.
- 988 Suicide & Crisis Lifeline: Dial 988 for immediate help in a mental health or substance-related emergency.
You’re not alone. The path to stability and renewal begins with a single, supported step.

 Written By:
Written By: Edited By:
Edited By: Clinically Reviewed By:
Clinically Reviewed By: 




 Verify Insurance
Verify Insurance